Birth control
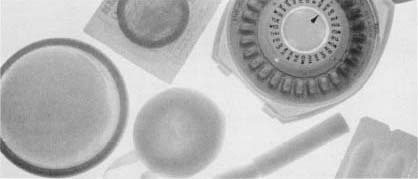
Birth control, also known as contraception, is the use of physical barriers, timing, chemicals, or a combination of the three to prevent pregnancy. The vast majority of contraceptive methods are designed for use by women. No method except abstinence (not engaging in sexual intercourse) is guaranteed to be completely effective. Used according to directions, however, most modern birth control methods are safe and effective.
Pregnancy prevention methods have existed in some form through-out history. The methods employed have varied widely, with the religion, culture, and scientific sophistication of each society helping to determine the types of birth control used. In the twentieth century, birth control advocates such as Dr. Marie Stopes (1880-1958) in the United Kingdom and Margaret Sanger (1879-1966) in the United States fought prevailing religious and cultural taboos in order to provide information and supplies to anyone who wanted them.
Surgical Birth Control Procedures
Female tubal ligation ("tying the tubes") involves cutting the fallopian tubes (either one of two slender tubes that carry eggs from the ovaries to the uterus), and burning, clipping, or banding the severed ends. Since fertilization of the egg takes place in the fallopian tubes, a tubal ligation prevents pregnancy from occurring. Tubal ligation can usually be performed as outpatient (short-term recovery) surgery and is sometimes performed as an immediate postpartum tubal ligation (in the period of time just after a woman has given birth).
Male vasectomy involves severing the vas deferens, the two tubes that transport sperm from the testes to the ejaculatory duct. Since semen thereafter contains no sperm, impregnation cannot occur. A vasectomy is also an outpatient procedure. Some questions have been raised about the procedure's long-term health effects, but the prevailing medical opinion is that vasectomy is unlikely to cause any health problems. Both tubal ligation and vasectomy can be reversed in some cases but generally are considered permanent.
Oral Contraceptives ("The Pill")
Birth control pills contain various amounts of the female hormones estrogen and progesterone that mimic the natural condition of pregnancy, when a woman normally cannot become pregnant. The first contraceptive pill was developed in Massachusetts by endocrinologist Gregory Pincus (1903-1967), biologist Min-Chueh Chang (1908-), and physician John Rock (1890-1984). The pill contained progestin, a synthetic progesterone developed in Mexico by American chemist Carl Djerassi (1923-). In 1960 it was approved by the U.S. Food and Drug Administration (FDA) and first became available by prescription under the name Enovid (produced by G.D. Searle & Company.)
Though questions have arisen about their long-term safety and possible links to certain forms of cancer, oral contraceptives are considered appropriate for many women when used under medical supervision. They are the most popular form of contraception and are used by 28 percent of women of childbearing age. Also contributing to their popularity is their high rate of effectiveness.
Long-Lasting Hormonal Contraceptives
Norplant, produced by Wyeth-Ayerst Laboratories, is a device containing a form of progesterone in six tubes the size of matchsticks. These tubes are surgically implanted under the skin. The tubes prevent pregnancy by gradually releasing progesterone over five years. Norplant was approved by the FDA in 1990, though questions have been raised about possible links to cancer, as well as concern about certain side effects, including weight gain, depression, and headaches.
Depo-Provera, produced by the Upjohn Company, is a synthetic form of progesterone that is used in almost 100 countries. One injection works for three months. FDA approval was withheld in the 1970s because of possible links to cancer and osteoporosis. In 1992 the FDA once again began the process of approving Depo-Provera.
Intrauterine Device (IUD)
An intrauterine device (IUD) is placed within the uterus for long-term prevention of pregnancy. It is not known precisely how an IUD prevents conception, but it is believed to produce uterine irritation, causing an inflammatory (fiery, severe) tissue reaction that is toxic (poisonous) to sperm and blastocyst (embryonic tissue).
Modern IUDs date back approximately 100 years. Today's devices, made of plastic, copper, or steel, are formed into loops, coils, and T-shapes. An IUD must be inserted and removed by a physician. Some IUDs have been associated with conditions like perforation (puncture) of the uterus, pelvic inflammatory disease, and even death. A. H. Robins' Dalkon Shield, an IUD design no longer manufactured, is notorious for its high complication rate. At least 20 deaths and thousands of internal injuries have been blamed on its use.
The most successful IUD is the plastic Lippes loop, developed in the 1960s by Dr. Jack Lippes (1924-). The device is straightened and placed in a tube for vaginal insertion into the uterus, where it resumes its loop shape when the tube is removed. Threads attached to the IUD extend into the vagina, so the user can check that the IUD is still in place and has not been expelled. Most contemporary IUDs are variations of the Lippes loop, containing either copper or progesterone.
Condoms
A condom is a latex rubber or lambskin sheath (covering) placed over the erect penis to trap the semen (the fluid containing the sperm) ejaculated (discharged) during sexual intercourse. The condom also helps prevent the spread of venereal disease (sexually transmitted disease, or STD). The condom is the only method of birth control that also decreases the transmission of such diseases as hepatitis, AIDS, and papilloma virus, which is responsible for cervical cancer (cancer of the cervix, the narrow end of the uterus). The practice of using condoms during intercourse dates back to at least the sixteenth century. A condom can be used with or without spermicidal foams or gels.
Diaphragm
Developed in Germany in the late nineteenth century, the diaphragm is a flexible rubber barrier that a woman inserts into the vagina before inter-course. The diaphragm covers the cervix (the narrow end of the uterus that leads into the vagina) to prevent sperm from entering the uterus. The diaphragm is an effective means of birth control when used in combination with a spermicide. Diaphragms come in different sizes, and a woman must be fitted by a birth control expert to get a prescription for the correct size.
Spermicides
Beginning in the 1970s spermicides, chemicals such as nonoxynol-9 that kill sperm, became available in suppositories, foams, creams, jellies, and sponges. Inserted into the vagina before sexual intercourse takes place, spermicides may be used alone or may be combined with condoms and diaphragms for greater effectiveness.
Male Contraceptives
For the first time in over 100 years, there is news to report in the field of male contraceptives. Two studies have been using the hormone testosterone to suppress (lower) sperm production. An injectable form of the hormone is featured in World Health Organization (WHO) research, and an oral form is being used by the University of Washington (Seattle) in association with researchers in Bologna, Italy.
Both groups succeeded in lowering sperm production enough to qualify for the WHO's definition of infertility. The WHO study, conducted over two years with men in four continents around the world, showed the injections to be 98.6 percent effective in preventing pregnancy, which is similar to the effectiveness of birth control pills. Sperm counts for the men in both studies returned to normal after the hormones were stopped, proving that the treatment is reversible (the men could later father children).
These studies are exciting because they prove that it is possible to create an effective male contraceptive. The University of Washington study also proves that oral hormones can suppress sperm counts, which was not thought to be possible (researchers believed a concentrated pill form would be toxic). But researchers still predict a long wait—maybe even 50 years—before the male pill will be available.
Selective Abstinence
Preventing pregnancy using the rhythm method requires a woman to carefully track her monthly cycle, so she can avoid engaging in intercourse near the time of ovulation. The rhythm method is the only method of birth control accepted by the Roman Catholic church. The temperature method (developed in 1947) involves monitoring body temperature variations during the monthly cycle. Temperature falls below normal in the weeks before ovulation, drops further during ovulation, and then rises above normal until menstruation. Monitoring variations in the quality and quantity of vaginal secretions can also help pinpoint the ovulation time. The calendar method assumes that ovulation consistently occurs on the fifteenth day of the monthly cycle, and is subsequently highly ineffective.
Comment about this article, ask questions, or add new information about this topic: